Kidney Allocation
How are donated kidneys offered to people on the wait list?
There are over 200 people waiting for a kidney transplant in Manitoba right now. To make sure allocation of donations take place in a fair and transparent manner, the Kidney Allocation Policy was first developed in 2008 with many partners including Transplant Manitoba.
The policy explains what happens when a donor kidney becomes available for transplant. Updates were made in 2016 to reflect changes in national standards, advancing technology and new transplantation data.
Additionally in January 2016, the province of Manitoba introduced donation after cardio-circulatory death (DCD) which allows more families to consider organ donation. Organ donation after cardiac death makes it possible for organs to be donated after the heart stops beating. Offering organ donation after cardio-circulatory death is expected to increase donation rates by 20 to 25 per cent.
Key points
Definitions
Medical need means dialysis therapy alone is not available or not enough to maintain health or life.
Utility means the best possible post-transplant outcomes must be considered to improve patient and transplant results, and reduce the need for a second kidney transplant.
Justice means ensuring everyone who is on the wait list for a transplant has a fair chance of being transplanted.
How do the changes in policy affect me?
The policy change better balances those on the wait list by making sure:
- Children and adults on the deceased donor kidney list receive the best kidney for them.
- People who are not highly sensitized receive a transplant based on how long they have been on dialysis and how well they match.
Frequently asked questions and answers
What do these changes mean?
- Children will be transplanted quicker.
- Enhanced matching between donor and recipient will improve long-term outcomes.
- People who are highly sensitized and difficult to match will have a better chance of receiving a transplant.
- Introducing the Kidney Donor Profile Index (KDPI) ensures evaluation and allocation services benefit all recipients.
How was this policy formed?
Transplant Manitoba participated in a National Consensus Forum with other Canadian transplant programs, the Kidney Foundation of Canada, as well as legal and ethical experts to develop a clear set of key points that would guide how decisions are made for patients on the wait list for a kidney.
Transplant Manitoba organized focus groups for patients on dialysis and waiting for a kidney transplant to learn how they understood the rules and to ask questions about what a fair system for kidney allocation in Manitoba would look like.
Focus groups told us:
- Patients have little knowledge on how donor kidneys are allocated and the requirements necessary to be on the wait list.
- Patients expect the wait list and allocation rules to be transparent and fair.
- Patients agree with ranking patients based on set rules.
- Patients expect that the allocation rules to be fair.
- Patients want the allocation rules to be readily available to all patients.
- Patients want the allocation rules to be explained to them in plain language.
- Transplant Manitoba developed a clear set of kidney allocation rules for all Manitoba patients on the wait list using the feedback and learnings from the National Consensus Forum.
What principles guided the development of the Kidney Allocation Policy?
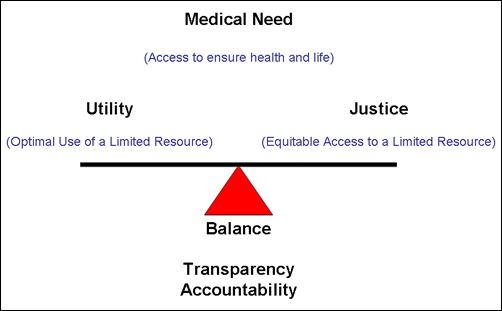
The key principles are medical need, utility and justice. These principles can compete with one another, so striking a balance is essential. For example, medical need may give more priority to a patient with a short wait time ahead of a patient with a longer wait time.
This balance is anchored by two important pieces - a transparent system developed with input from key people, including patients, and accountability to ensure the process is monitored and checked regularly.
How were medical need, utility and justice used to determine process?
Medical Need
- Inadequate Dialysis
For patients who are no longer effectively dialyzed because peritoneal and hemo dialysis are no longer possible or work well, a transplant becomes a life-saving therapy.
- Children
Medical evidence shows that a kidney transplant has an increased benefit for children. A kidney transplant can help youth to properly grow, develop and learn. Therefore children are given a high priority for receiving a kidney transplant.
Utility
- Tissue (HLA) matching
The better the tissue match between the donor and recipient, the better the chance that the kidney transplant will last longer.
- Young kidney to young recipient
A kidney from a young donor can last for many years. This means that giving a young kidney to a young recipient maximizes the donor’s gift.
Justice
- Wait-time on Dialysis
To ensure fair access, priority increases for patients based on their wait time from the date dialysis treatment started.
- Sensitization Level
Patients are “sensitized” if their immune system has made antibodies against potential donor kidneys making donor compatibility difficult. As people become more and more sensitized (from pregnancy or blood transfusions) the compatible donor pool becomes smaller and it takes longer to find a donor match. To ensure fair access, when a compatible donor is available, priority will be given to that person. However, it is important to remember that at a very high level of sensitization (80% or more) it may take years to find a compatible donor.
- Prior Living Kidney Donor
While very rare (less than 0.5% of all living donors), these people may need a kidney transplant themselves. Having already donated a kidney, it is fair that they get some priority when a donor kidney becomes available.
How do medical need, utility and justice work together to set allocation rules and rank patients on the wait list?
The following system assigns priority for patients waiting for a kidney transplant:
|
Overriding priority Inadequate dialysis |
| High priority Children Previous kidney donor |
| Normal priority *KPDI < 20 KPDI 20 – 59 KPDI 60 – 95 Patients < 60 All patients Patients ≥ 60 Priority score = wait-time score + tissue match score + sensitization score(1 point/year) (up to 3 points) (up to 1.9 points) |
| No priority Pre-emptive transplantation |
* KDPI stands for Kidney Donor Profile Index. It is used to as a tool to ensure patient safety, equitable access and the best use of donor kidneys for all recipients.
Highest level - Overriding Priority
These patients are given the next available compatible donor kidney.
Up to 15% of all kidneys are allocated for these types of patient.
High Priority
These patients are given the next available compatible donor kidney as long as there are no “Overriding Priority” patients listed.
Up to 10% of all kidneys are allocated for these types of patients on the wait list.
Normal Priority
These patients are given the next available compatible donor kidney as long as there are no “Overriding or High Priority” patients listed.
Most (at least 75%) donor kidneys are allocated to patients who fall within this group. To ensure a fair allocation for the “Normal Priority” group, a priority score is used.
The patient with the highest number of points will have top priority for the donor kidney. The priority score is based on:
- the total of the points accumulated for wait time on dialysis (1 point per year)
- the level of tissue (HLA) match (to a maximum of 3 points)
- the level of sensitization (to a maximum of 1.9 points)
To best use the limited number of donor kidneys, a “young donor to a young recipient” rule is in place. This reduces the need for a younger recipient to be re-transplanted in their lifetime and ensures fair access for all patients on the wait list – more people on the wait list will be seeking just their first transplant. It is important that the young donor rule not disadvantage older patients – older recipients maintain “Equal Access” to a kidney transplant. Transplant Manitoba has introduced two major safeguards:
- The definition of a young donor applies only to people under the age of 25.
- A kidney from an older donor (60 years of age or more) is only offered to a recipient 55 years of age or older.
No Priority
These patients are not on dialysis, but have significant kidney disease that is likely to lead to the need for dialysis. These patients may be transplanted with a donor kidney before the start of dialysis only if there are no other compatible patients with a higher priority level. This happens very rarely.
How does Transplant Manitoba ensure accountability and transparency to the public?
Transplant Manitoba formed the Kidney Review Committee based on feedback from dialysis patient focus groups. The Committee’s main role is to hold the transplant programs accountable and ensure transparency for all patients.
Kidney Review Committee mandate:
- Conduct audits of all donor kidney allocations to ensure the rules are being followed.
- Review the kidney allocation rules every year to make sure that the rules are achieving the goals of fairness and equality.
- Start and oversee a formal process for allocation rule updates that is transparent and done in consultation with patients.
Kidney Review Committee membership:
- WRHA Ethics Medical Officer – Chair
- Transplant Manitoba – Program Manager – Vice Chair
- Patient Representative (Kidney Recipient Advocate) x 2
- Patient Representative Officer, HSC Winnipeg
- Social Work Representative
- Manitoba Renal Program Representative x 2
- Transplant Manitoba Program Representative
- Key Public Stakeholder
The medical directors of the kidney transplant programs report all kidney allocations to the Committee.
Contact us
If you have more questions, or would like to provide feedback to Transplant Manitoba please contact us.








